5.5.19 is international day of the Midwife and my blog is dedicated to all Midwives who have made a difference by defending a woman from any unnecessary intervention – be that anytime related to pregnancy 🤰🏾 antenatally , during any kind of birth or postnatally.
I’ve decided to share three stories which are true experiences written by midwives about defending women. One of the stories is mine but I won’t say which one .
As clinical midwives we are seen as equal members of the huge maternity wheel alongside women and their families, managers, obstetricians, future midwives , maternity support workers and many more – although in reality there is a hierarchy that many within our own discipline and other disciplines are striving to challenge and change .
The truth in plain sight is that just one member of the team is not engaged or equally involved (including the woman) then the intricate workings of the mechanism will be disrupted.
Women and families = get to know your midwife/midwives . Ask questions , be curious. Read books that are informative, recommended and that explain your bodies and your babies abilities with balance and clarity . Try the Positive Birth book by Milli Hill Click HERE to see on Amazon (founder of The Positive Birth Movement) . 
Prepare yourself as much as you can. Don’t leave any stone of knowledge or information unturned . Join a positive birth group Click here to find out more . Be aware that midwives are defenders of women – talk to other women and find the midwife that helps you to believe in yourself . You’ll know when you’ve found her – don’t settle for second best. I believe women should rock the boat of maternity services like pregnancy pirates. Try reconnecting with midwife from a previous birth if you have other children – it’s evidence that continuity pf carer will reduce your chance of interventions so ask to see the same midwife at your appointments. Look at the birth statistics of your local units and choose wisely – ❤️ The Which birth guide is a good resource although might need updating Click HERE to view

Managers = be insightful of how staffing levels and skill mix will impact positively or negatively on birth outcomes – when you arrive to help us in our hour of need ask not what we can do but show us what you can do to improve our shift . Stay curious ❤️
Obstetricians = be mindful of the physiology of the female form and how your positive or negative behaviour will impact on the delicate balance of all hormones involved in playing out the birth process . Watch midwives working see them as equals . Stay curious ❤️.
Midwives = be aware of why you are a midwife. Embrace your role as not to
“do to”
but to
“be with”
to defend,to stand up for ,to support, to strengthen and to keep safe. Unite the team with your passion for all births❤️. Stay curious
Maternity support workers I am thankful for you all – you do support ❤️- your gratitude towards the midwives that make the toast and tea for the family and ensure rooms are left clean before transferring women from them . (we do ask other midwives to follow our suit) as we know you always have work to do within the scenes and behind them – running the operating theatre, birth-room turnaround time , restocking , clinical work, bringing the team together , being aware of all areas . The camaraderie and team work you display so strongly within your discipline is a benchmark for us all . Stay curious
❤️❤️❤️❤️❤️❤️❤️❤️❤️❤️
Three stories of defending
Read on reader ….
Story one
The elective premature Caesarean birth – a courageous Midwife
All eyes upon me , the baby is only 34 weeks old . The mother’s instinct to hold her newborn is tangible I hear her breath . The paediatric team stand around the resuscitaire , prepped , ready, waiting and impatient. Something inside me tells me “give the baby to the mother , give the baby to the mother” After delayed cord clamping I cocoon the newborn in a warm towel without touching and within seconds I’m helping the mother with her first embrace. Time stands still. I monitor the baby closely but without words for colour , breathing , heart rate (with my stethoscope) tone and reaction , a saturation monitor on the baby’s right hand (pre-ductal) reassures me. All is good . I offer to take photos of mum dad and baby, mum and baby , baby’s hands touching mum , many photographic variations evolve in so little time . I look across at the paediatrician- she knows me, trusts me – she smiles at me and nods mouthing “it’s ok” . Five or more minutes have passed – mum knows it’s time . Dad carries his newborn to be seen by the team . Mum is crying not with sadness but with joy that hers was the first skin to touch her newborns , then her partners – this is how every new beginning of life should be – we Midwives must step aside but wait in the wings ready to prompt or assist- our silent presence is reassuring to the family ❤️
It was all worth the fear – afterwards I hug the paediatrician and say “thank you for trusting me ” the mother scrolls through her photos in disbelief that her only ever precious child started its journey against her skin – I am a defender ❤️
Story Two
The “Failed” Induction challenging a decision
“Can I help ?” I offered “Oh great” replied the ward Midwife “we are so busy!! Can you go with the consultant to see the woman who’s Induction didn’t work ?”
I’d been sent from labour ward to help on the antenatal area . The consultant was counselling an elderly primigravida ( over 45 years old) . The woman “Joy” (false name) was being told that two attempts at induction and due to her age that a caesarean would be for the best . I was sent to get the consent sheets . I’d just completed the AQUA shared decision making course and I was keen to put what I’d learnt into practice.
The time on the clock was 16.55 so bear that in mind .
What happened next was that the consent forms were handed to the woman after the risk of Caesarean was explained . The woman dutifully signed the consent forms and the consultant left the department. Something inside me told me this didn’t feel right . My instinct and experience made me go back to the woman and her partner. I asked them if they were okay with everything. In fact I went as far as saying “are you okay about your Caesarean birth?” They both voiced their concerns but felt they haven’t been given a choice. I wanted to discuss further so I went to the phone and rang the consultant to return . The phone call did not go well -the consultant was quite irked that I’d phoned told me to check the clock and to ring the consultant on call.
I rang the on call consultant who came and discussed further the choices the woman had with her and her partner . She opted for an attempt at labour following artificial rupture of her membranes which would all take place on the labour ward .
To cut a long story short the woman progressed to 5cm dilatation and remained there . She was very pleased with the fact that she’d experienced labour and been listened to . Her caesarean birth was a positive unhurried experience.
A few weeks later I came face to face with the first consultant one my day off – I’d come into work to attend a two hour study session . The consultant openly criticised me in front of a new senior registrar who I’d never met before – belittled springs to mind . “Thank you for overruling my decision to plan a Caesarean without labour” were the words. I stated clearly that the best way to clarify the situation was to determine how the woman felt – “are you invited to the naming ceremony of the baby ?” I asked “no” was the consultant’s curt reply – “well here’s my invite” I said (by coincidence I’d found it in the staff mail box that day) . The consultant went quiet and walked away . I am a defender ❤️
Story Three
Rebalancing the birth hormones
I met Nasrit about one hour into my shift in the morning. (name changed) . The community midwives has brought her in because her labour had slowed then stopped. Nasrit was having her third child, she lived with anxiety and panic attacks which were inherited from her childhood . My opinion was that her fear had disrupted her birth hormones – I discussed this with her – she held my hand tightly . I went to the midwives station and put Nasrit’s name on the board – as I did I could hear staff chipping in “does she need an ARM?” “Get the syntocinon running when the Reg arrives ” “is she actually labouring ?”
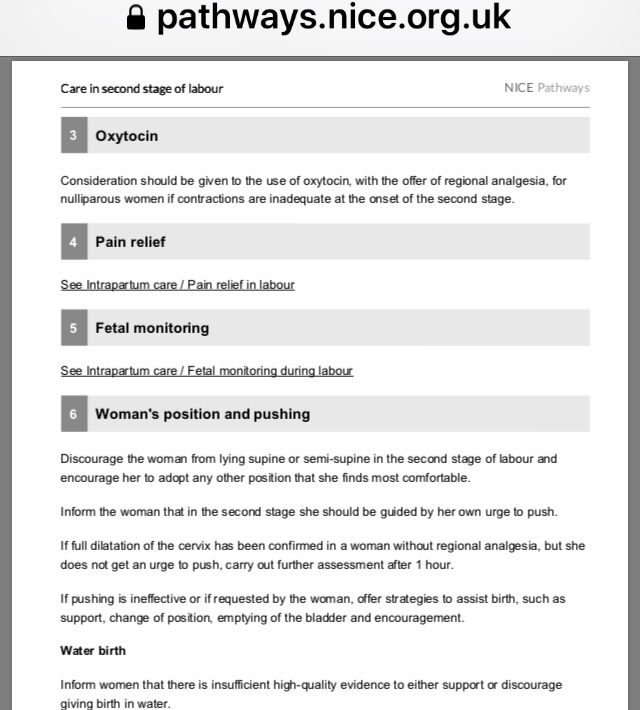
I pretended not to hear the comments . I was going to go back to Nasrit, Nasrit’s partner and Nasrit’s mother . My plan was to try and get Nasrit into a birthing state of mind . I wanted to make her at home. In giving her possession of her room I made her space – no lights , quiet , no interruptions and a haven for her birth . I keep a set of battery powered fairy lights in my locker and I’m trained to use aromatherapy. My key goals were to make sure I had everything in the room that Nasrit needed and nothing in the room that anyone else needed -there were going to be no interruptions. I used a blend of lavender and frankincense in hot water as a room infusion. I explained to Nasrit how aromatherapy would work. I then turned off all the lights and switched on the fairy lights . As an equal I explained to Nasrit and her family how relaxing can help oxytocin and that anxiety can hinder by producing cortisol and adrenaline . Nasrit was with me . I sat and held her hand (at her request ) we all waited without talking . I reiterated that there was no pressure . It took about 15 minutes for Nasrits heart rate to drop from 96 to 68 – she was breathing more calmly .
Over the next two hours Nasrit’s labour recommenced and soon she was holding her newborn skin to skin . I never left the room .
All was well
I am a defender ❤️
Summary
So the reason for my blog is for you to try and reflect on your own practice as a midwife and find those times when you were a defender. Look to see when you recognise fellow defenders through their words and actions . Try not to ask “does this feel right for the woman ? ” “is the woman’s face reflecting agreement or disagreement ”
Stay curious and keep defending
❤️We are defenders❤️
#IDM2019
Post script dedication I’m dedicating this blog to all midwives in hardship – whether physically, emotionally or financially. The Cavell Trust is a charity that helps nurses , health care assistants , maternity support workers and midwives Click HERE for more information

Thank you for reading my blog .
Yours in midwifery love
JennyTheM ❤️
Stay curious
and like Professor Lesley Page (@Humanisingbirth on Twitter) be the leader of the dance ❤️❤️







 Midwifery cannot be like predictive text eg this is the way we do it , this is the length of time you need to help a woman, new offspring & partner postnatally before transfer to the ward and so on .
Midwifery cannot be like predictive text eg this is the way we do it , this is the length of time you need to help a woman, new offspring & partner postnatally before transfer to the ward and so on .