Today is an exciting day for me . I have just registered a new hashtag that I hope will influence every woman and midwife . The hashtag is
#BirthLeadership ©️
As a midwife one of my aims is to display leadership towards women in order to support them through their labour and birth . I hope that this cascades onto future midwives so that they too can show leadership. This process may involve eye contact , holding hands , a hand on a shoulder , researching,debating decisions, reading information, challenging the system BUT together as a team to help make women feel like they are the leaders of their own births . Whatever the mode of birth it’s right that midwives let go and give the lead control to the woman . This can be through education and sharing views but first and foremost it must be about midwives listening to women’s hearts, voices, dreams and plans.
Midwives begin by championing women’s choices so that birth is given back to women .
Sheena Byrom OBE and Professor Soo Downe of UCLAN co-wrote an research article called “She sort of shines” Click here for PDF 
in Box 1 as above the midwives interviewed were asked about the connection between leadership identifying commonalities between both .
The huge psychological impact of having no voice in a birth is well documented and can have long term physiological effects on a woman’s mental health . Studies on post birth PTSD (Post traumatic stress disorder) often highlight the lost voice of the woman and her fear of speaking out .
Birth leadership is created so that every midwife questions her own practice in order to ask herself “am I displaying birth leadership skills?” – in other words “what am I giving to this woman and her birth to relinquish my control and give her the lead in her own birth”
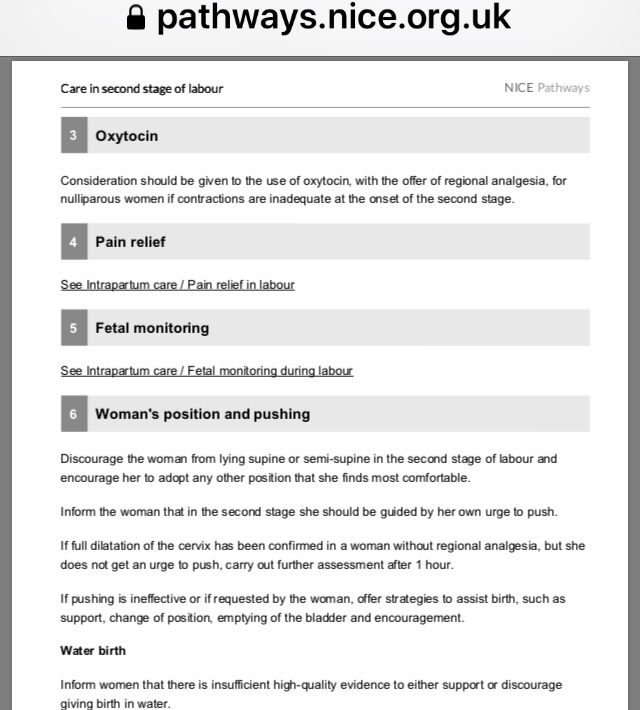
Let’s take for example coached pushing in the second stage of labour something which is neither evidence based practice or conducive to effective care – yet still it goes on. Click here for NICE guidance in 2nd stage of labour April 19
Some midwives FOLLOW this tradition and their fear of changing practice influences others negatively, preventing birth leadership in some NHS maternity units.
We must become champion challengers and this doesn’t mean loudly-it can be quite subtle and indeed this quiet way is less likely to disrupt a woman’s oxytocin flow – promoting both a sense of security and safety .
Let’s talk optimal cord clamping – and how Amanda Burleigh knew in her midwifery bones that immediate cord clamping wasn’t quite right – it didn’t sit well in her midwifery skin- @OptimalCordClamping showed Birth Leadership and started to challenge research and change practice which led to optimal cord clamping (OCC) being included on NICE guidance – Quality statement on OCC Amanda’s Birth Leadership is ongoing and she has inspired others to talk about OCC by inspiring them for example Hannah Tizard who is @BloodToBaby on Twitter . This is true practice change for women and babies . Here’s Amanda’s twitter feed .
The way you act in and out of work shows the person you really are . Your aim should always be to help others as much as you’d help yourself – keep that formula equal every minute in your midwifery career and you won’t go wrong .
Women need to know we care ❤️
Try and wear a new pair of glasses when you go into work – sit in a different chair for your lunch , ask colleagues “what are my good and bad habits?”, question your usual behaviour and remember why you became a midwife – to give the lead to women.
Birth leadership is about small steps or huge steps beginning with the next woman you are with as she gives birth .
If you have shown birth leadership of any kind use #BirthLeadership and tweet about it
Here are a few Birth Leadership examples
SkinToSkin in the operating theatre
Not weighing a baby until after it’s first feed
Leading a woman to change position in the second stage to avoid lithotomy
Helping a woman to birth and hold her stillborn baby and making the family a safe space ❤️
Helping a woman who has been constantly monitored on CTG to the bathroom for a walk and a wash
Being silent as a woman is in the second stage of labour
Supporting a woman compassionately through a difficult birth
Helping a woman to avoid unnecessary internal examinations
Being a baby’s advocate when the woman is having a GA Caesarean
Holding a woman’s hand in an emergency situation
Caring for a woman’s relatives as well as the woman herself
Here is an uplifting reply from @FWmaternity co-founder of MatExp and inspiring obstetrician who is supportive of Midwives and promotes her Trusts home birth team ❤️
NB please don’t think this about starting a campaign yourself although that would be great it’s about sharing the little things that signify BirthLeadership to inspire change – so please add yours on Twitter ❤️
Thank you for reading
Yours in Birth leadership love
Jenny ❤️
PS
Please add your comments to my blog – I welcome all feedback
❤️Facilitate what is happening rather than what you think ought to be happening. If you must take the lead, lead so that the mother is helped, yet still free and in charge. When the baby is born, the mother will rightly say, “We did it ourselves!”
Tao Te Ching – ancient Chinese quote about what being a midwife means ❤️

 Midwifery cannot be like predictive text eg this is the way we do it , this is the length of time you need to help a woman, new offspring & partner postnatally before transfer to the ward and so on .
Midwifery cannot be like predictive text eg this is the way we do it , this is the length of time you need to help a woman, new offspring & partner postnatally before transfer to the ward and so on .