There is so much written about discharge planning for Care of the Elderly / Unscheduled care / patients requiring rehabilitation .
Currently there are extra pressures on maternity services and I have set out my objectives as to why I want to discuss postnatal discharge planning below
1.To highlight beacons of positivity
2.To inspire discussion
3. To make discharge planning an intrinsic part of the admission process
4. To identity where a same day transfer should not be promoted
5. To make the actual ‘time of discharge’ a governance issue
6. Share good practice and eliminate bad practice
7. Raise the profile of effective discharge planning in maternity services
I have learnt from others and by listening to families how the NHS could streamline the discharge process I’m certain that this would make a positive impact on staff time , families understanding , effective communication , reduce complaints and develop a well rounded understanding of the discharge process.
Going home with a newborn is seen as an easy and smooth process so my blog will try to help parents as well as midwives and maternity workers to see that this is not always the case.
The best time to be discharged home is in the morning , however the pressure on postnatal wards is immense and they have one of the fastest turnovers in the NHS . So often we hear of women and newborn being sent home at ridiculous hours and HERE is an article about this in Mother and Baby
So how can we streamline the discharge process ?
A. Find out if the family have transport home
B. Start the discharge paperwork by checking address and phone number are correct
C. Ensure medication to take home is requested as soon as possible
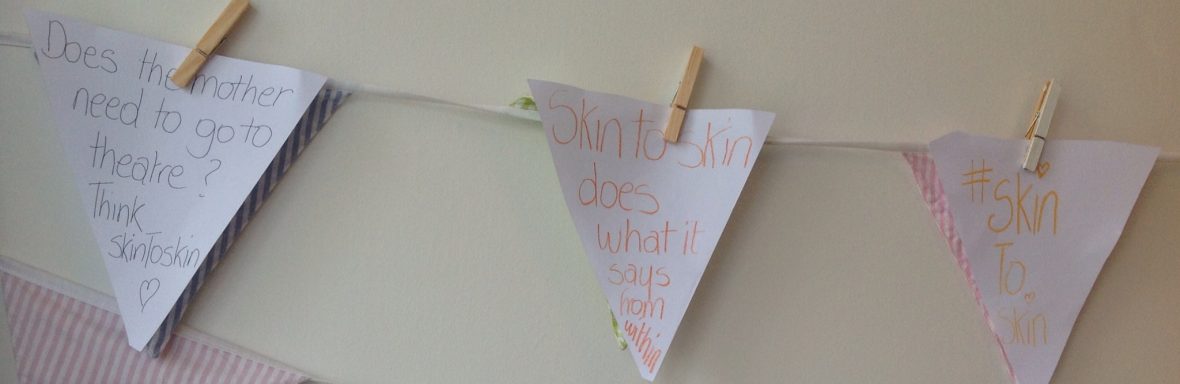
D. Promote and explain why prolonged skin to skin contact will ensure not only breastfeeding success but also maternal and newborn wellbeing and that continued skin to skin contact is important as well as talking to the newborn and feeling calm (it’s crucial to discuss co-sleeping and I usually direct parents to ISISSLEEP as well as explaining – I’m not going to go into depth about this now, but I do with parents.
E. Ask about support at home – visitors who come and help are very valuable and aid recovery and coping . At the same time it’s important that the new family have some time alone in order to gain confidence in being new parents and learning to recognise various cues that their newborn makes .
F. Go through thoroughly signs and symptoms of illness for mother and baby and mention sepsis – any infection caught early improves the outcome.
G. Ensure all levels of midwifery staff are competent to discharge women and babies home – in busy times when there are pressures on the service this will facilitate an “all hands on deck” situation
H. Employ a discharge facilitator who can assist clinical staff to organise the paper trail
I. Have a generic checklist to refer to primarily so that women and families can see what the process entails and secondly so that staff do not miss any of the steps involved and this will avoid mistakes and maintain communication at all levels .
J. The first point of contact in regard to any queries should always be the labour ward and / or community midwife . Midwives are responsible for postnatal care up to 6 weeks post birth – I am proud to say that when women present at labour wards they are seen quickly – a walk in centre or a triage service are not equipped to deal with postnatal care – midwives are .
Explanation, discussion , allowing time and two way communication are all integral to a successful discharge process . I like to tell families that the discharge is in effect a transfer of care to the community midwifery team and also what to expect from the visit. Midwives do not expect families to be up , dressed and ready with the house perfect – they are visiting to see how families are feeling and coping . To assess if the baby is feeding well and to give support .
Rushing the process because of pressure has no value and affects communication in a negative manner – it’s so valuable to discuss why discharging takes time at antenatal group and have information on discharge at clinic appointments .
Ideas such as group work on the postnatal ward to increase questions and save time are being developed in various NHS trusts and discharge guidelines should be updated regularly to match the process.
Talking about safe regular analgesia and how to take medication will improve recovery , reduce infection , help mobility and be key to reducing venous thromboembolism . Perineal pain is real – it hurts – but in the first day it may not be as bad until the woman arrives home and starts to question her pain threshold . Pain management is part of postnatal care and can make the difference between good recovery and feeling awful for days .
Perinatal mental health care is gradually improving and it takes skill and experience for midwives to recognise it if the woman is reluctant to disclose . Continuity of carer and knowing ones midwife makes talking about postnatal depression and anxiety easier – but we still have a lot of work to do . HERE The Guardian highlights perinatal anxiety . Post Traumatic Stress Disorder is now a recognised illness caused by trauma around birth – communication and compassion at birth can reduce this and I recently received a letter from a woman telling me that skin to skin contact helped her to cope during an emergency situation – so there’s something to consider . I am proud to know Emma Sasaru who has PTSD and courageously BLOGS in order to help other mothers to recognise the signs and how to seek help .
As the midwife completing the discharge YOUR responsibility is also to ensure the baby is feeding and that you have observed a feed and given the mother support. Talking about maintaining milk supply and support groups as well as how to recognise that the baby is thriving must be discussed . It’s just as important to explain and know the family understands how to make up milk if the baby is not being breastfed.
The neonatal examination is not a future prediction of health it just says the baby is fine at the moment it is done . Any signs like continuing sleepiness, a very quiet baby , poor muscle tone and slow weight gain might be indicators of poor health – mothers usually have an instinct about these things so listen well and get the baby seen by a paediatrician – don’t manage the baby at home without senior input .
Finally time of discharge is an issue – do families reall want to go home at 23.00 or 3am ? It’s a personal choice but CHOICE it must remain there is no place for sending women and newborns home in the middle of the night – does it happen in any other department? I have never heard of children being sent home in the night or elderly patients so why should we accept it for women or maternity services? If you have concerns that families are bring sent home at inappropriate times there is action you can take – escalate it to your line manager , fill out an incident form , discuss at your team meeting and raise with your governance lead. Ask other units what they do and be pro-active .
The main point I want to get across is that discharge from hospital is a complex process . It is much more effective when there is two way communication between midwives / obstetricians and families . Talking about going home must start as soon as the admission process starts. Discharging someone home must be a high quality , thorough , kind and efficient task. It must also be individualised and embody compassionate care . Use your skills in effective discharge and teach them to future midwives – it’s important to share good practice.
I hope I have raised your interest in discharge planning . I appreciate and value all feedback and understand there may be some points I have missed . My main aim is to promote thought , discussion and change .
❤️Thankyou for reading
Love Jenny ❤️